December 8th 2025
Get Healthy Utah staff had the opportunity to attend the inaugural Growing Stronger Communities: Sustainable Agriculture for Nutrition Security in Raleigh, North Carolina. It was hosted by Inter-Faith
November 14th 2025
Get Healthy Utah, together with the Utah League of Cities and Towns, is pleased to announce that three Healthy Utah Communities have earned their redesignation this fall: Ephraim, Layton, and North Sa
October 17th 2025
Get Healthy Utah, together with the Utah League of Cities and Towns, is excited to recognize five new Healthy Utah Communities this fall: Bountiful, Cedar City, Cottonwood Heights, Midway, and Murray.
September 24th 2025
Get Healthy Utah held its Annual Event this September at the Viridian Event Center in West Jordan. This year’s theme was “Fueling Healthy Communities,” with a focus on access to healthy food. Leaders
June 24th 2025
From August 2023 to December 2024, West Valley City’s Healthy West Valley Committee took part in the Active People, Healthy Utah Demonstration Project. This project, funded jointly by Get Healthy Utah
April 28th 2025
Get Healthy Utah, in conjunction with the Utah League of Cities and Towns, is pleased to announce the newest Healthy Utah Community designees. Five cities and towns qualified this spring: Koosharem, P
March 5th 2025
On February 5, 2025, the Utah Business of Health Event, organized by Get Healthy Utah, The Utah Worksite Wellness Council, and Utah Community Builders, took place at the Loveland Living Planet Aquariu
January 16th 2025
Key Takeaways:
Generally, there is a strong correlation between social connection and positive health outcomes
Social connections may be protective against heart disease–related deaths
Social
December 16th 2024
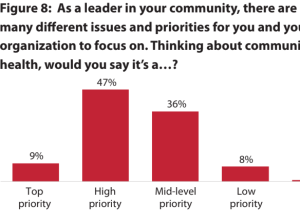
Get Healthy Utah worked with the Kem C. Gardner Policy Institute to learn more about city and town leaders’ attitudes and strategies regarding the Healthy Utah Community Designation and community heal
October 21st 2024
This fall, Get Healthy Utah partnered with Move Utah and Bike Utah to host the first-ever Connected Communities Summit! The summit, which was held September 18-19, 2024 at the Utah Valley Convention C
August 28th 2024
Implementing a Milers Morning Program in Schools
Written by Susanne Creer, Physical Education Specialist at Terra Linda Elementary School
Milers is a voluntary morning before school walk/jog progr
July 18th 2024
This spring, Get Healthy Utah partnered with the Utah Foundation and Guiding Our Growth to host the first-ever Healthy Communities Roadshow! The roadshow, which ran from March to May 2024, consist
May 31st 2024
Alysia Ducuara
Alysia Ducuara is the Executive Director for Get Healthy Utah.
Springtime means conference and event season at Get Healthy Utah! From visiting with our parks and recreation champion
April 30th 2024
Trilby Cox
Trilby Cox is Co-Executive Director for Bike Utah, a Utah-based nonprofit. Bike Utah is partnering with Get Healthy Utah and Move Utah for the Connected Communities Summit this fall.
Bi
April 18th 2024
The Healthy Utah Community designation is valid for three years. To qualify for redesignation, communities must complete the following:
Submit a new letter of commitment
Continue to hold health
April 18th 2024
Get Healthy Utah, in conjunction with the Utah League of Cities and Towns, is pleased to announce the newest Healthy Utah Community designees. Six cities and towns qualified this spring: Mapleton, Ore
March 14th 2024
Get Healthy Utah partnered with the Utah Worksite Wellness Council and Utah Community Builders to host the second annual Utah Business of Health Event! The event took place on February 7th, 2024 at th
March 7th 2024
Chet Loftis
R. Chet Loftis is the Managing Director of PEHP Health & Benefits, a public sector health plan that covers over 170,000 members. He is also the new Board Chair for Get Healthy Utah.
Go
January 17th 2024
Morgan Hadden
Morgan is the Program Coordinator for Get Healthy Utah. She graduated from Utah State University with a B.S. and M.P.H in Health Education and Promotion.
Chances are, your city or t
January 2nd 2024
Greg Bell
Greg Bell is the outgoing Get Healthy Utah Board Chair. Greg previously served as president of the Utah Hospitals Association and lieutenant governor for Utah.
In 2014, a group of us cre
November 3rd 2023
Cindy Nelson
Cindy is an Extension Associate Professor in Beaver County Utah with responsibilities in Family and Consumer Sciences and 4-H. She loves the people she serves, and the variety of progra
October 17th 2023
Get Healthy Utah held its annual Stakeholder Retreat this October at the Viridian Event Center in West Jordan. This year’s theme was “Connection: Building a Culture of Health.” Topics included the con
September 26th 2023
Devynne Andrews, JD
Devynne Andrews is the Communications Coordinator for Get Healthy Utah.
Recently, the Get Healthy Utah staff attended an advance screening of UnCharitable, a documentary about
September 5th 2023
Get Healthy Utah, in conjunction with the Utah League of Cities and Towns, is pleased to announce the newest Healthy Utah Community designees. Four cities and towns qualified this fall: Coalville, Hol
August 4th 2023
Dr. Amy Locke
Amy Locke is the Chief Wellness Officer for the University of Utah Health, executive director of the University of Utah Health Resiliency Center, Professor of Family and Preventive Med
July 31st 2023
Elisa Soulier
Elisa Soulier is the Vice Chair for the Get Healthy Utah Board. She works as Director of Health and Wellbeing at Castell. She focuses on delivering more high value holistic care for pa
July 17th 2023
Jennifer Porter and Rachel Bowman
Jennifer Porter, RDN, is a Health Program Coordinator, and Rachel Bowman is a Nutrition Coordinator for the Utah WIC program. Visit wic.utah.gov to learn more.
Nu
July 11th 2023
Key Takeaways:
“Green streets” have more plants, soil, and water-friendly systems than traditional streets
Originally, green streets were designed to capture rainwater locally
Green streets al
June 28th 2023
The Utah Foundation recently released a report, Healthy Communities: Advancing Wellness and Safety, focused on policy solutions for Utah communities to increase physical activity. The report is meant
June 9th 2023
Get Healthy Utah held its annual Advisory Council this May. We want to thank everyone who attended and shared their ideas on how we can improve healthy eating and active living in Utah through system-
May 16th 2023
Key Takeaways:
Utahns are in a mental health crisis and need the healing and social connection that arts and culture can deliver.
The arts foster connection, support the healing process, and com
April 24th 2023
Get Healthy Utah, in conjunction with the Utah League of Cities and Towns, is pleased to announce the newest designees of the Healthy Utah Community award. Six cities and towns qualified this spring:
April 19th 2023
Kathleen Britton
Kathleen Britton, SNS has served as the Director of Child Nutrition Programs at the Utah State Board of Education, since February 2014. Ms. Britton began her nutrition work as a Die
April 10th 2023
Kimberly Clevenger
Kimberly Clevenger is an Assistant Professor in Kinesiology and Health Science at Utah State University, with a background in exercise physiology. Her research interests are in th
March 25th 2023
Greg Bell
Greg Bell is the Get Healthy Utah Board Chair. Greg is president of the Utah Hospitals Association, and previously served as lieutenant governor for Utah.
Recent research in Great Britai
February 27th 2023
This February, Get Healthy Utah and the Utah Worksite Wellness Council held the Utah Business of Health event, with the theme “Good Health is Good Business.” Leaders from Utah businesses and insurance
October 28th 2022
Get Healthy Utah held its annual Stakeholder Retreat this October in Salt Lake City, with the theme “Building Healthier Communities.” A variety of leaders attended to learn more about their common
August 3rd 2022
Organization: Get Healthy Utah
Contact: Alysia Ducuara, Executive Director
Location: 2180 S 1300 E, Suite 440, Salt Lake City, UT 84106
Program Details:
The mission of Get Healthy Utah is to c
July 14th 2022
In June 2022, Get Healthy Utah offered mini-grants to cities and towns that want to provide their citizens with better opportunities for healthy living. Cities and towns could apply for up to $5,000 t
October 13th 2021
Each year, Get Healthy Utah gives Partnership Awards to organizations that have collaborated across sectors to significantly improve community health. This year at the Fall 2021 Get Healthy Utah Stake
October 13th 2021
The Fall 2021 Get Healthy Utah Stakeholder Retreat was held in-person on October 7th in Salt Lake City. Attendees represented various sectors that have an upstream impact on community health, such as
August 1st 2021
On June 30, 2021, Get Healthy Utah held a virtual information session on type 2 diabetes, the National Diabetes Prevention Program (National DPP), and the importance of Medicaid coverage. During the i
June 2nd 2021
The Annual Get Healthy Utah Stakeholder Retreat was held virtually on May 5, 2021. The event focused on the One Utah Roadmap. Lt. Governor Deidre Henderson provided the keynote address. The closing s
March 10th 2021
What is a wellness policy?
A wellness policy creates a safe and healthy environment for students and staff to practice lifelong healthy habits. The school community (which includes parents, students
November 3rd 2020
Social and economic conditions where we live, work, and play can impact our health status. These include income, affordable housing, safe places to walk, healthy food access, discrimination, and healt
August 20th 2020
Get Healthy Utah is proud to have partnered with Comagine Health, Intermountain Healthcare, Utah Department of Health, and University of Utah Health to host the free virtual summit for worksites Impro
August 4th 2020
Jeff Hummel, MD, MPH Medical Director, Health Care Informatics, Comagine Health Meredith Agen, MBA Vice President, Health Care Analytics, Comagine Health
The COVID-19 pandemic has seemed both distan
June 20th 2020
Guest Post by Brett McIff
Brett McIff, PhD is the Physical Activity Coordinator for the EPICC Program at the Utah Department of Health. His research has focused on the perception of the built envir
April 21st 2020
Rural communities often have poorer health outcomes than non-rural communities. This is due, in part, to barriers to accessing healthy food, opportunities for physical activity, and mental health reso
April 15th 2020
A new, and timely, report from the Utah Foundation examines trends and challenges related to teleworking. Findings include:
Teleworking seems to have a positive effect on productivity and employee
March 24th 2020
Gyms, recreational facilities, schools, and extracurricular activities are cancelled. While we are all doing our part to stay home and maintain proper social distancing, it is important to be physical
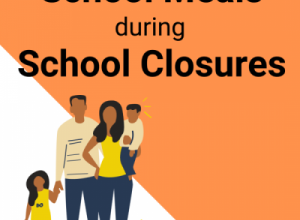
March 18th 2020
To help in preventing the spread of COVID-19, Utah schools are dismissed for a soft closure until March 27th.
What does this mean for school meals?
On average, 50% of Utah K-12 students participat
February 20th 2020
Guest Blog Post By, Kate Wheeler, Child Nutrition Specialist, Utah State Board of Education
Kate works on farm to fork and local procurement initiatives. Kate has an MPH from Emory University. Prior
January 14th 2020
The Utah State Board of Education has provided Best Practice for Recess Guidelines. While not mandated, the guidelines support the Utah State Board of Education’s Strategic Plan Safe and Healthy Schoo